Medical Imaging Relevant to Scoliosis Care
Today we’re talking imaging – medical imaging – breaking down what types of images we use for diagnosis and treatment of those with scoliosis and kyphosis.
X-Rays
X-rays are one of our oldest forms of medical imaging – they were discovered in 1895 by a professor of Physics in Bavaria. He discovered them accidentally while testing whether cathode rays could pass through glass, and because he did not know what these rays were, he called them “X” for “unknown.”
He won the 1st Nobel Prize in Physics for this discovery in 1901, and X-rays rapidly became both widespread and unrestrained until the 1940’s, with shoe stores routinely offering X-rays so customers could see the bones in their feet! There was little regard for the side effects of radiation exposure during this time.
There are many positive attributes of X-rays: they’re quick, they’re cheap, and they are actually the gold standard in visualizing scoliosis, as X-rays provide clear imaging of the bones and the bony alignment of the spine via electromagnetic radiation.
Scoliosis study X-ray
In fact, the most important image we look at in the scoliosis world is called a Scoliosis Study, which is an X-ray image of the entire torso, taken in a standing position, from the jaw down to the hips.
This should be ordered as standard practice for anyone with scoliosis, but unfortunately, that isn’t always the case. Physicians with less experience with scoliosis often order X-rays of just one part of the spine, for example, just of the lumbar spine (lower back).
This gives an incomplete picture of the scoliosis, as it’s important to visualize any counter-curving happening above or below the main scoliosis, as well as the overall trunk balance — which means where the head is in relation to the pelvis.
The Current Procedural Terminology (CPT) Code for a Scoliosis Study X-ray is 72082, which means “Radiologic Exam, Spine, Entire, 2 or 3 views”.
We at SchrothDC prefer 2 views: the Anterior-Posterior (AP) view, as well as the sagittal view. In the state of Virginia, where we practice, you’ll need a doctor’s prescription to have X-rays taken. You can ask your general physician or any specialist you’re seeing for a prescription for CPT Code 72082, or you can ask your doctor to fill out this prescription referral form.
Let’s loop back around to that unrestrained X-ray-ing of the first half of the 20th century — what happened to all those repeat shoe store customers who had their feet routinely X-rayed? Or the doctors who devoted their lives to using and studying X-rays with their patients?
Many truly terrible things, mostly due to lengthy X-rays (think 30-minute to 2-hour exposure times compared to 10 seconds present-day). I won’t list them here, but it pretty much sounds like the last 30 seconds of modern-day pharmaceutical ads when they tick off all the potential side effects of the drugs just after telling you how great and life-changing they are.
Instead, let’s focus on the one side effect of radiation that we are most considerate of today, cancer. We now know that repeat exposure to radiation can cause certain types of cancer — for scoliosis patients, the risk is most pronounced to the reproductive organs and the breasts, as those areas of the body are exposed to radiation while capturing the image of the spine.
A study done by National Cancer Institute following 5,000 women with Adolescent Idiopathic Scoliosis found that this group had a 70% higher chance of developing breast cancer than the general population.¹ Because kids and teens need X-rays of their spines every 4-6 months during periods of growth (the group mentioned above had a mean number of 24 X-rays during their course of treatment), we should really be considering the collateral damage of this frequent radiation exposure.
Luckily, as a species, we evolve over time, and in 1992, another professor of Physics discovered a new type of X-ray detector that gives off a much lower dose of radiation than a conventional X-ray: 50-80% less. He also won the Nobel Prize in Physics. This newer x-ray technology is called EOS, and is highly recommended for kids and teens with scoliosis to minimize their radiation exposure while being treated for scoliosis.
EOS machines are expensive, so unless you live near a cutting-edge Children’s Hospital or in/near a metropolitan area, you may find yourself without access to this option. If this is the case and you or your kiddo must have conventional X-rays, ask the tech for lead pads for the reproductive organs and the breasts to shield those areas from radiation.
We are lucky to have access to an EOS machine in the office we rent space from, the National Scoliosis Center (NSC). Many of our patients, kids and adults, will opt to have their X-rays taken at NSC for less radiation exposure and the ease of transferring the images to us at SchrothDC.
Okay, so we’ve managed the first imaging hurdle for scoliosis and kyphosis; now what? For anyone under the age of 18, there’s one additional X-ray needed to provide information regarding skeletal maturity, or in simpler terms, how much growth a child or teen has left. This next section does not apply to adults.
Bone Age Study: Risser Sign vs. Sanders Score
Once scoliosis or kyphosis has been diagnosed in a child or teen, we need to know as medical professionals (and as parents), “What is the risk of progression?” or in other words, “How worried should I be?”. The risk of scoliosis and kyphosis progression is based on how much growth a child has left. There are two ways to determine this, both via X-ray.
Risser Sign
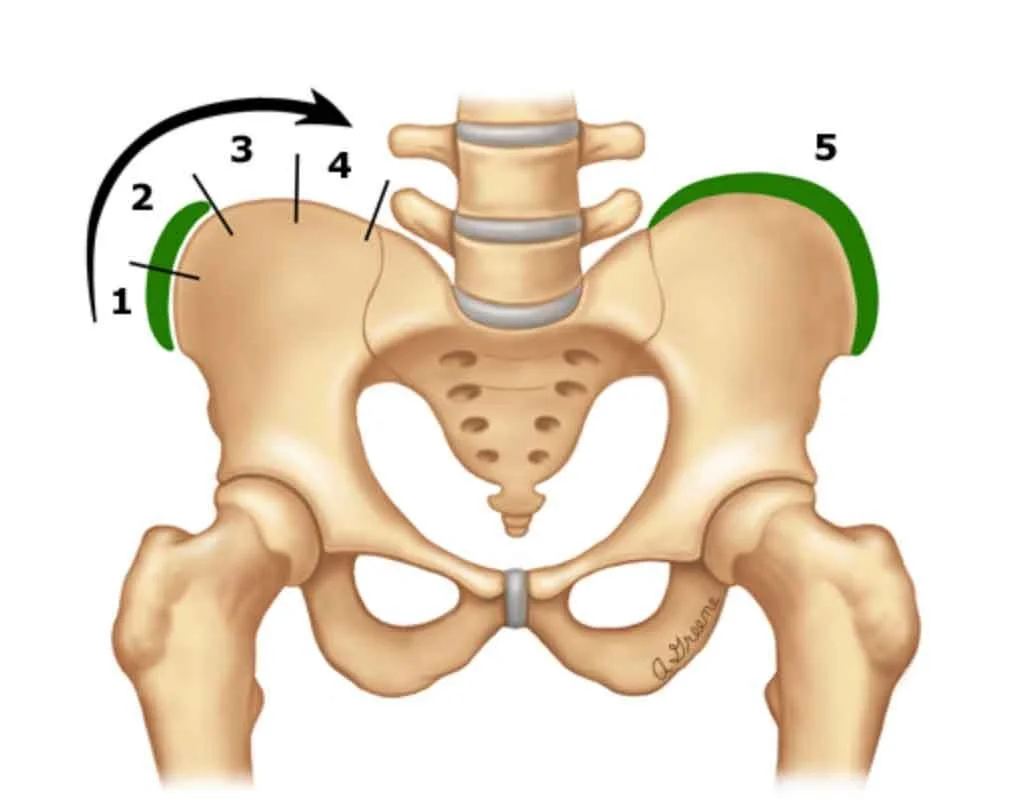
Risser Sign Diagram
The first, the Risser sign, determined by looking at the X-ray of the hip bone, has been used since 1958.
Risser Sign via X-ray
The grading system for Risser is 0–5, with 0 being the least skeletally mature and 5 being fully skeletally mature. This system was used as standard practice until 2011, when Sanders simplified skeletal maturity scale was developed and became the new status quo of measuring skeletal maturity.
Sanders Score
Sanders Skeletal Maturity Scale
Sanders requires an X-ray of the hand, preferably the left, due to the high incidence of non-dominance and, therefore, less trauma or deformity on that side.
The scale ranges from 1–8, with 1 correlating to “juvenile” or skeletally immature and 8 correlating to mature. Many in our field now prefer Sanders over Risser due to Sanders being simpler, more reproducible, having a substantial correlation with the curve acceleration phase, and being a good predictor of peak height velocity.²
Sanders Hand X-ray
If you are the parent of a child or teen diagnosed with scoliosis or kyphosis who has not discussed skeletal maturity with your kid’s physician yet, this is the time to start asking questions and getting clear answers, as your child’s skeletal maturity will dictate treatment.
Here’s what to ask:
What is my child’s Risser Sign? This can be determined from their Scoliosis Study X-ray.
What is my child’s Sanders Score? If the doctor has not yet taken a hand X-ray, request it. It’s CPT code 77072, “Bone Age Study, Hand, 1 View”
Based on my child’s Risser Sign and Sanders Score, what is their risk of progression? We’re including a cheat sheet for you here to determine the risk of progression based on the Risser and the Sanders
Risk of Progression Chart
Should my child be wearing either a night brace or a full-time brace due to their risk of progression?
I truly don’t enjoy being the bearer of bad news, and I swear I am actually a very optimistic person, but…pediatric and adolescent scoliosis cases are mismanaged ALL. THE. TIME.
I evaluated a 17-year-old patient last week who had been instructed to wear a brace from age 13–15, at which point the doctor said he was done growing and assured mom it was okay to discontinue the brace, and since that time, his curve has progressed from 20 degrees to 30 degrees. Mom is livid with that doctor, and I can understand why.
This particular doctor does not specialize in adolescent scoliosis and gave the family really bad advice. Unfortunately, this is not an outlier case. Scoliosis is still poorly understood in most of our modern medical system — the best thing you can do as a parent or a patient is seek medical professionals specializing in scoliosis and kyphosis.
The next few images we discuss today apply to special populations, not everyone with scoliosis and kyphosis will need these next three.
Leg Length Discrepancy X-Ray
Limb Length Study X-ray
If anyone on the medical team — physician, orthotist, or physical therapist — suspects that a scoliosis patient has one leg longer than the other that may be impacting their scoliosis, we will often request a “Limb Length Study,” CPT code 77073 (Bone Length Study).
This is an x-ray, in standing, from the hips down to the feet. The long bones of the legs are then measured digitally and compared left to right.
A leg length discrepancy of more than 1.5cm is considered significant and may need to be treated. We treat leg length discrepancy on a case-by-case basis, most often with a lift inside of the shoe for discrepancies under 1cm and by professionally lifting the entire sole of the shoe for discrepancies over 1cm.
Kids tend to compensate well for leg length discrepancy and rarely need to be lifted, whereas adults often develop symptoms related to the discrepancy and can benefit tremendously from a proper lift.
DEXA Scan
This section applies almost exclusively to older adults: women over the age of 50 and men over the age of 65. A dual-energy X-ray absorptiometry, or DEXA Scan, assesses bone density. It tells us if we have normal, dense bones, osteopenia (lowered bone density), or, worst-case scenario, osteoporosis (bone density so low that we are at risk for fractures).
Scoliosis and Osteoporosis are not a good combination, as lowered bone density fuels scoliosis progression. For women, menopause often reduces bone density, which is why we often see scoliosis progression in post-menopausal females.
Men don’t tend to lose as much bone density until after age 65 due to a steady decline in sex hormones. This is when we are likely to see scoliosis progression in males. For any adult with known scoliosis or an adult recently diagnosed with scoliosis, a DEXA scan is a must-do beginning at the ages listed above, depending on your gender.
It helps us predict the risk of scoliosis progression in adults and allows us to incorporate recommendations for general exercise, dietary intake, and pharmaceutical recommendations to slow or halt the loss of bone density. Read more about bone health and scoliosis in our previous blog post.
MRI for a Left Thoracic Scoliosis
A left-sided scoliosis in the thoracic spine (the mid-back) is atypical and often, but not always, associated with other serious medical diagnoses. Chiari malformation, in which brain tissue extends into the spinal canal, and Syrinx, a fluid-filled cavity within the spinal cord, are highly associated with a left-sided thoracic curve.
If this type of curve is present, especially when paired with an abnormal neurological examination, referral to MRI (magnetic resonance imaging) of this area is standard practice to look for the above diagnoses.
MRI’s for Disc, Joint, and Nerve Issues
MRI’s are not standard practice for diagnosing and treating scoliosis — they are seldom used for children and should be used sparingly for adults. They’ve been around since the 1970s and help visualize the soft tissue components of the spine (think ligaments, discs, nerves, and spinal cord).
The downsides are that they are expensive, lengthy, and loud! However, when spinal symptoms become more than just garden-variety muscular pain, referral to MRI is common.
MRI’s are indicated when a patient has weakness, numbness, abnormal reflexes, and/or pain in the legs, a non-movement-related pattern of spinal pain, or chronic spinal pain. Most typical are MRI’s of the cervical spine (neck) and lumbar spine (low back), as those areas are more vulnerable to disc herniation, joint degeneration, nerve compression, and stenosis.
These soft-tissue problems can occur as scoliosis progresses due to the natural aging process, also called degeneration, so MRI’s certainly have their place in the scoliosis world. We at SchrothDC often reference the 1–2 page written summary of our patients’ MRI’s to inform us of any significant nerve, disc or joint impairment.
Medical Imaging Takeaway
As you digest this large amount of medical information, remember no one needs every single one of these tests. Try to stick to the sections that apply to you — your age group, your gender, and your symptoms.
If you’re visiting us at SchrothDC, you only need a scoliosis study X-ray to start. We’ll guide you through this complex medical system that we live in, advising you on the next steps. We’ve got your backs, literally.
References:
1. Ronckers C et al. Cancer mortality among women frequently exposed to radiographic exams for spinal disorders. Radiat Res. 2010 Jul; 174(1): 83–90.
2. Chazono M & Obata S. A Simplified Skeletal Maturity Scale and Thumb Ossification Index to Assess Skeletal Maturity and Predict Peak Height Velocity in Japanese Females with Adolescent Idiopathic Scoliosis. Spine Surg Relat Res. 2021; 5(4): 244–251.