Bone Health and Scoliosis
If you are one of the many kids, adolescents, or adults living with and managing scoliosis, the importance of the health and strength of your bones cannot be overstated – we need to talk people!
Let’s start from the beginning and with the basics. Our youth is a time when we build bones. Until our early 20s, we are making new bone faster than we are breaking down old bone, which leads to an overall net increase in bone mass. (This process of breaking down and building up is normal: bones are in a constant state of renewal.). Around age 30, we achieve peak bone mass.
How do we build bone?
The physical therapist (PT) in me is jumping up and down with joy waiting not-so-patiently to answer this question: exercise, exercise, EXERCISE!!!
To keep it simple, exercise, any type, requires the contraction of our muscles. Muscles contract, pulling on the bones that they attach to, and this “pulling” stimulates extra deposits of Calcium and nudges bone-forming cells into action.
So what does this mean for our youth: our kiddos, our teens, our young adults…?
The more bone mass we attain in youth, the less likely we are to develop a bone density deficiency issue (i.e. osteopenia or osteoporosis) later in life.
As I watch my twin two-and-a-half-year-olds sprinting, skipping, jumping, and climbing, I’m realizing (maybe for the first time, I’m embarrassed to admit) the importance of this physicality for their bones. Being a PT, I’ve always had a close eye on their muscle development and their motor skills, but I’ve truly never thought about their bone development. The twins need this physical activity to burn the endless amounts of energy they have, but they also need this, physiologically, for their bones to become stronger at this stage in life.
One of the many jobs of parenting is setting our kids up for success when it comes to exercise. When they are very young, bringing them outdoors and to the playground, as well as giving them time to explore different environments to test out motor skills is key. As they age, signing them up for a variety of sports to try is a great way to keep them active as well as social with their peers. As your child progresses to adolescence, well, good luck…
Although some teens are natural jocks and get plenty of exercise, there is a large subgroup of teens who become sedentary around puberty. These teens are notoriously hard to motivate (I can sense parents’ nodding heads as I write this.) I won’t proclaim to know exactly how to motivate a sedentary teen, but here are some ways I try as a therapist:
Encourage them to find a type of exercise that interests them in some capacity, and doesn’t feel like “work”. Just because their peers feel connected to mainstream sports or weightlifting doesn’t mean your teen will. Maybe your teen will find connectedness with something abstract, like archery or fencing, or something incredibly anti-contact/anti-competitive, like yoga, or even walks around the neighborhood with a friend. Anything and everything counts when it comes to physical activity - even spontaneous dance parties in the living room.
Lead by example. If you as the parent aren’t demonstrating consistent healthy exercise habits, it’s hypocritical to expect your teen to do so. So much of parenting is modeling behavior that your kids are picking up on subconsciously.
Make sure they know that regular exercise doesn’t have to be a set amount of time per day, or even consecutive minutes of exercise. An active healthy lifestyle could be a short walk in the morning, swimming with friends in the afternoon, and some stretching before bed. Exercise by no means has to be sweating profusely for an hour minimum while sucking wind. Most sedentary teens would never find that enjoyable. Plus, research shows that lifelong exercisers tend to engage in shorter but more frequent spurts of exercise, and also view 5-minute opportunities to exercise just as valuable as 60-minute opportunities.
If you are parenting a child or teen who has scoliosis, this exercise discussion becomes even more pertinent. There is a moderate amount of research that suggests that teens with scoliosis who progress to a surgical range (Cobb Angle greater than 50 degrees) have concordant osteopenia or decreased bone mineral density.¹,² The hypothesis is that decreased bone mass/density may cause severe scoliosis progression in teens.
What we’re aiming to achieve is the highest level of peak bone mass as we approach and reach age 30, because after age 30 we begin to lose bone mass faster than we create it. Remember, the more bone we get into our “bone bank account” by age 30, the less likely we are to develop osteopenia or osteoporosis as we age.
The second most common time in life that we see scoliosis progression (other than puberty), is during and after menopause (for women), and between the ages of 65-70 for males - this is a direct result of decreasing bone density. Because of the profound drop in the hormone estrogen during menopause, women can lose bone rapidly starting around age 50. Estrogen slows the natural breakdown of bone, so when levels fluctuate, and then plummet, bone loss and therefore bone density deficiencies can develop rather quickly. Males’ hormone levels wane more gradually over a longer period of time, which is why bone density issues won’t appear until later on, around age 65. This is typically a “silent” process: there are no signs or symptoms that your bone density is decreasing - no pain, and often no fractures right away. Thus, receiving an Osteopenia or Osteoporosis diagnosis can be shocking.
How is Osteopenia and/or Osteoporosis diagnosed? When should you be screened for it?
A simple, non-invasive test called a dual-energy X-ray absorptiometry, or DEXA Scan, assesses bone density. It’s important to note that your primary care will not begin to routinely order this test for you until you reach age 65. Given what we know about scoliosis progression in menopausal women, we encourage all of our female patients with pre-existing scoliosis to request a DEXA Scan beginning at age 50. The National Osteoporosis Foundation recommends having a DEXA scan at least every 2 years.
For men, screening is even less routine, as Medicare covers DEXA Scans in only limited circumstances for this gender. There is certainly a gender gap when it comes to bone health screening and care for men, even though 2 million of the 10 million Americans with Osteoporosis are male. For any of our male patients with pre-existing scoliosis, we request they begin getting DEXA Scans at age 65. For more information about osteoporosis risk for men, read this.
How do I Interpret my DEXA Scan results?
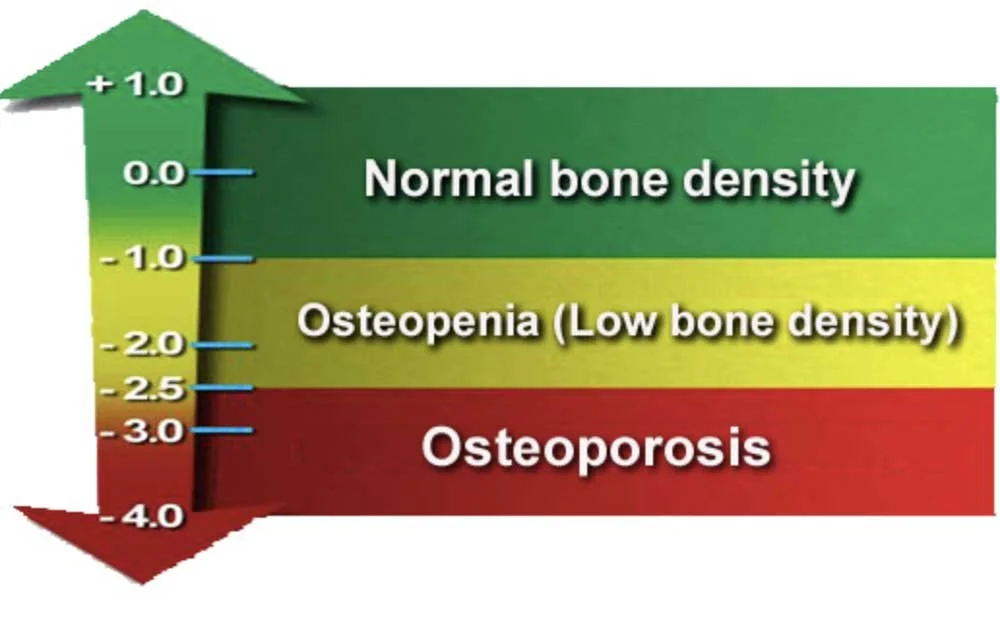
The hip, the spine, and sometimes the wrist will be scanned during a DEXA Scan. You will be given a “T-Score” for each part of the body scanned. If your T-Score is -1.0 or greater, your bone density is considered normal. If your T-Score is between -1.0 and -2.5, you have low bone density i.e. Osteopenia. If your T-Score is -2.5 or less, you have Osteoporosis, even if you have not yet broken a bone.
T-Score Chart
How does decreased bone density correlate with scoliosis progression?
Decreases in bone density, known medically as Osteopenia and Osteoporosis, mean a formerly dense bone is becoming porous. Think of sea coral or a pumice stone – instead of solid material, there are more holes, nooks, and crannies. Bones that have lost density are becoming more brittle, more fragile, and even “soft”.
Normal v. Osteoporotic Bone
Sometimes even a formerly straight spine can become scoliotic if the bone loss is severe enough – the porous structure of the bone can simply no longer hold the spine upright; it begins to curve to the side, and twist. I can’t tell you how many adults have come to see us stating “I never had scoliosis until age 55/58/60” – most of them post-menopausal women with no idea the correlation between menopause, bone density, and scoliosis. The incidence of scoliosis in the elderly (ages 65+) can be as high as 70%³, very likely because of decreasing bone density in that population.
What are the risk factors for developing Osteopenia and Osteoporosis?
Sedentary Lifestyle
Low Calcium Intake via Diet
Being Female
Being of White or Asian descent
Having a smaller body frame
Being post-menopausal
History of prostate and/or breast cancer (due to lowered sex hormones from treatment)
Long-term corticosteroid use
Medical conditions such as IBS, Celiac Disease, and RA
Excessive alcohol consumption & any tobacco use
As some of the above risk factors are out of our control – what gender or race we are, what previous medical conditions we’ve dealt with – we are left to focus on what is in our control.
Our lifestyle choices and how much we actively engage with life truly matters, no matter how old we are. Just because we’re not building bone after age 30 does not mean we should throw up our hands and lie down on the couch for our remaining years. You can start exercising regularly at any age, and at any level of fitness. Choosing appropriate activities and appropriate exercise intensity is crucial – this is something we love helping our patients with. An active, tailored-to-you lifestyle is always part of our Schroth Physical Therapy prescription. Even if you’ve been diagnosed with osteopenia or osteoporosis, exercise can help maintain bone density and prevent further deterioration.
Delving into this topic of healthy bones can take us in so many directions – from our discussion today regarding the importance of exercise, to best nutrition practices, and even to the use of pharmaceuticals to manage bone density.
Although nutrition and bone health deserves an entirely separate blog dedicated to the topic, I will say here that Calcium and Vitamin D are the two big players when it comes to healthy bones. We can ensure we’re getting enough Calcium by eating dark leafy greens – think kale, collards, and chard – as well as eating salmon, sardines, and soy products. Vitamin D improves the body’s ability to absorb the Calcium you’re eating, so make sure that you are getting sunlight exposure when possible, and eating up salmon (again) and trout. Vitamin D supplementation is also widely accepted by the medical community at this time.
Pharmaceutical management for osteopenia and osteoporosis? Also deserves its own blog post, BUT there is good evidence that anabolic bone density medication, such as Forteo and Tymlos, can help stabilize osteoporosis.
For now, we’ll keep the focus on moving our bodies to build and maintain strong bones – happy dancing, fencing, swimming, walking, kayaking, climbing, cartwheeling, skateboarding – the opportunities are endless!
References:
1. Burwell RG. Aetiology of idiopathic scoliosis: current concepts. Pediatr Rehabil. 2003;6:137–70. [PubMed] [Google Scholar]
2. Thomas KA, Cook SD, Skalley, et al. Lumbar spine and femoral neck bone mineral density in idiopathic scoliosis: a follow-up study. J Pediatr Othop. 1992;12:235–40. [PubMed] [Google Scholar]
3. Robin GC, Span Y, Sternberg R, Makin M, Menzel J et al. Scoliosis in the elderly: a follow-up study. Spine. 1982 Jul-Aug;7(4):355-9