What is Adolescent Idiopathic Scoliosis?
Most of our teenage patients here at SchrothDC have been given the diagnosis of Adolescent Idiopathic Scoliosis (AIS). It’s fairly common: out of 100 kiddos, approximately 3 of them will be diagnosed with it.
What is it? What causes it? What does it mean for the lifespan of the spine?
AIS involves a structural change of multiple vertebrae in the spine. Of all structural scoliosis, 75-80% is considered idiopathic. (Other types of structural scoliosis are neuromuscular, congenital, Recklinghausen, and Marfan or Beals-related. These types will be discussed in future blogs.)
AIS occurs equally amongst both males and females but is 8 times as likely to progress to the magnitude of needing treatment in females. Why? Females have earlier growth spurts, have unique hormonal factors during puberty that contribute, and achieve their final thoracic kyphosis shape later than males.
Let’s run though some definitions of Idiopathic Scoliosis – what it is and what it’s not. The Scoliosis Research Society (SRS), a society made up mostly of physicians, defines it as lateral curvature of the spine greater or equal to 10 degrees with rotation, of unknown cause. The Society on Scoliosis Orthopedic and Rehabilitation Treatment (SOSORT), made up of orthotists (i.e. the brace-makers), physical therapists, chiropractors, osteopaths, and physicians, defines AIS as a “Complex 3-dimensional deformity of the spine and trunk of unknown origin that involves rotation, lateral translation greater than 10 degrees, and collapse. It progresses during rapid growth, and appears in otherwise healthy children.”
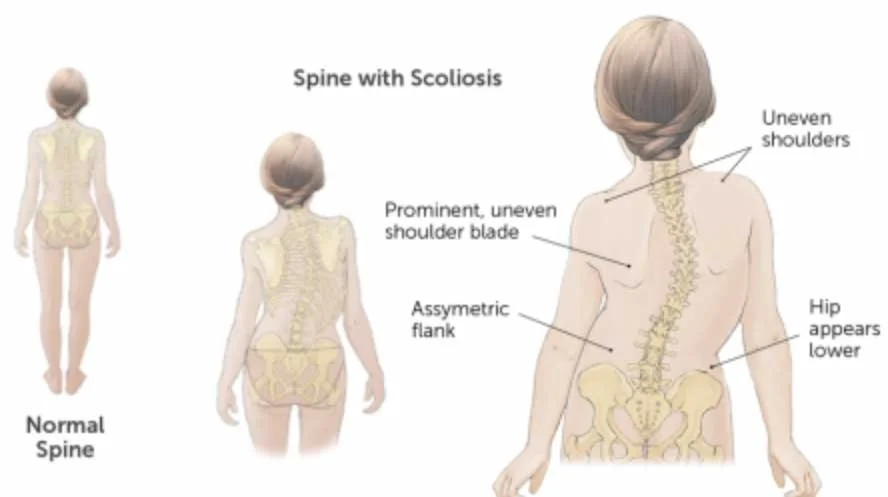
Typical Presentation of AIS
So that we are clear: 8 degrees of curvature on an x-ray = not idiopathic scoliosis (this could just be part of a person’s unique anatomy – one of many slight asymmetries that we all have). What about 15 degrees of curvature on a x-ray but without any appreciable rotation? Again, not idiopathic scoliosis. The latter example is likely what’s considered a secondary scoliosis, that is occurring secondarily to conditions like cerebral palsy, spinal cord injury, muscular dystrophy, and spina bifida – because we know the origin of that scoliosis, it can’t be idiopathic.) Knowing the difference is imperative in order to choose the best treatment, as well as to accurately predict future progression.
For those of you familiar with the term “idiopathic”, you already know that this blog will offer no clear-cut, proven answers on the origin of Adolescent Idiopathic Scoliosis, because the word idiopathic literally means a condition of unknown cause….
So we are left to speculate. Luckily, there are many professionals around the world who have dedicated their careers to the field of AIS: Dr. Rene Castelein, Dr. Manuel Rigo, Luke Stikeleather, and many more. They have put in countless hours studying this condition and the patients who are living with it.
Rene Castelein, an MD and PhD from the Netherlands, considers the genesis of AIS a “perfect storm”, where many factors come together in a short period of time, at or right before the growth spurt. His theory includes factors such as ligamentous laxity, less-than-optimal proprioception, changes due to maturation in the vertebral disc, and perhaps Leptin – a hormone secreted by fat cells to help regulate body weight, as adolescents with scoliosis consistently demonstrate lower body weight, lean muscle mass, and bone mineral density than healthy adolescent counterparts.
Luke Stikeleather, head of National Scoliosis Center , talks about “The 3 G’s” being determinants of AIS and subsequent progression.
Genetics – If a parent, sibling, aunt/uncle, or grandparent had AIS, there is a higher likelihood an offspring in that family will have it. It is likely a single gene disorder with dominant or recessive traits.
Growth – The more growth a child or teen has ahead of them at the time of diagnosis, the more risk of scoliosis progression, as the pubertal growth spurt is a time of high risk of AIS progression.
Gravity – We are all subject to the compressive effect of gravity. Kids and teens who are actively “fighting gravity” by playing sports and staying physically active most days will demonstrate less scoliosis progression than their sedentary counterparts.¹
Other theories regarding the origin of AIS include decreased melatonin, Vitamin D, and Calcium levels, but the studies on these concepts are not strong enough yet and more research needs to be done.
Historical hypothesis on the origins of AIS, including wearing heavy backpacks, being a ballet dancer, or playing an asymmetrical sport (like tennis), have never been proven in the literature. What we know now is that AIS is caused by genetics and systemic factors, not external factors.
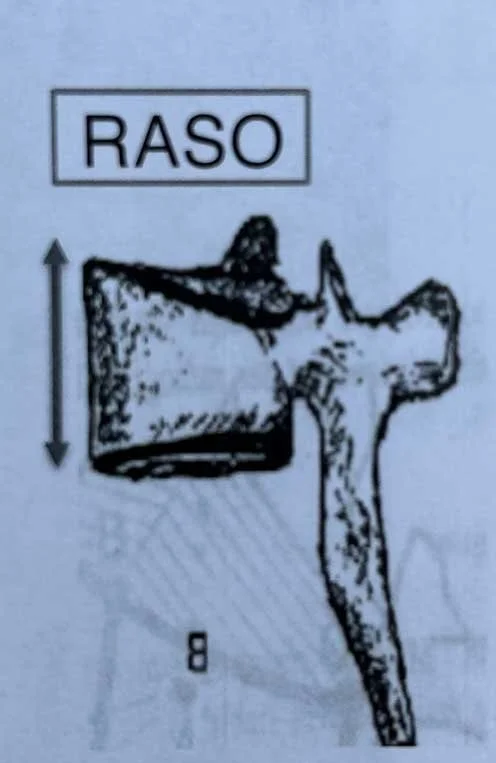
Now let’s loop back around to that “structural change in multiple vertebrae” we discussed before. However scoliosis initiates, what follows is vertebral deformity: the same vertebra deforms in all 3 planes of motion. In the sagittal plane, dorsal wedging is observed, meaning the anterior, or front, of the vertebra is wider than the posterior aspect. This is caused by a phenomenon coined RASO, an acronym for Relative Anterior Spinal Overgrowth.
RASO- Relative Anterior Spinal Overgrowth.
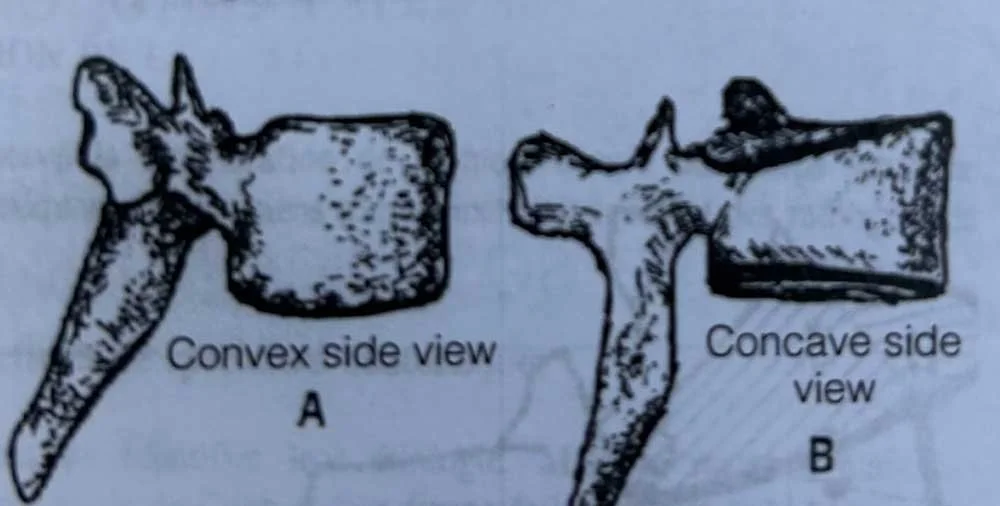
In the frontal plane, lateral wedging is observed, meaning the right side of the vertebra is wider than the left (or vice versa, depending on the direction of the scoliosis).
Lateral Wedging
In the transverse plane, intra-vertebral torsion causes deformation of the end plates of the vertebra.
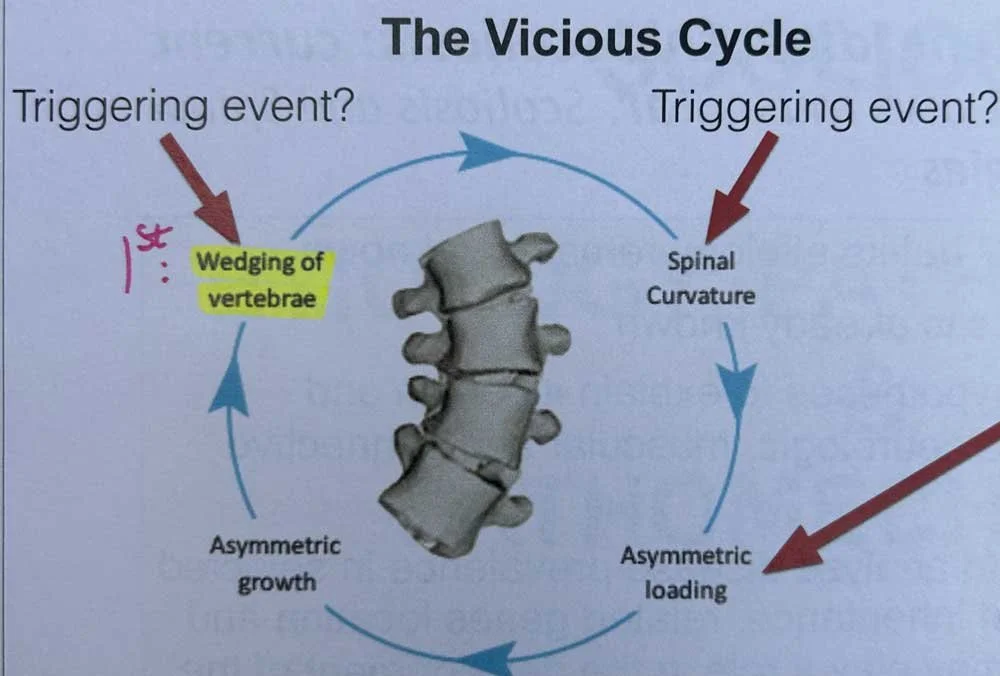
Although we don’t know for sure if the vertebral deformities cause the lateral curvature of the spine, or if the lateral curvature of the spine causes the vertebral deformities, Dr. Manual Rigo of Spain feels that vertebral deformity is primary. Once the vertebra deforms, the spine curves, beginning a vicious cycle of asymmetric loading (toward the convex side of the curve), which leads to more asymmetric growth, which leads to more deformity of the vertebra, which leads to more curvature of the spine, and on and on we go.
The Vicious Cycle
Most scoliosis professionals agree that the failure of the central nervous system to recognize this vicious cycle and control the asymmetries in the vertebra and spine are a large component of scoliosis progression, termed the Burwell Model of the Nervous System: Bi-Neuro-Osseous Timing of Maturation.²
This is where physical therapy for scoliosis comes into play (I know, I know, another plug for the Schroth Method, I couldn’t resist). Interruption of that vicious cycle is key, specifically the asymmetrical loading component. Physiotherapeutic Scoliosis-Specific Exercises (PSSE) incorporate cognitive, sensory-motor, and kinesthetic training to teach the patient to improve their posture based on the assumption that scoliosis posture promotes curve progression.
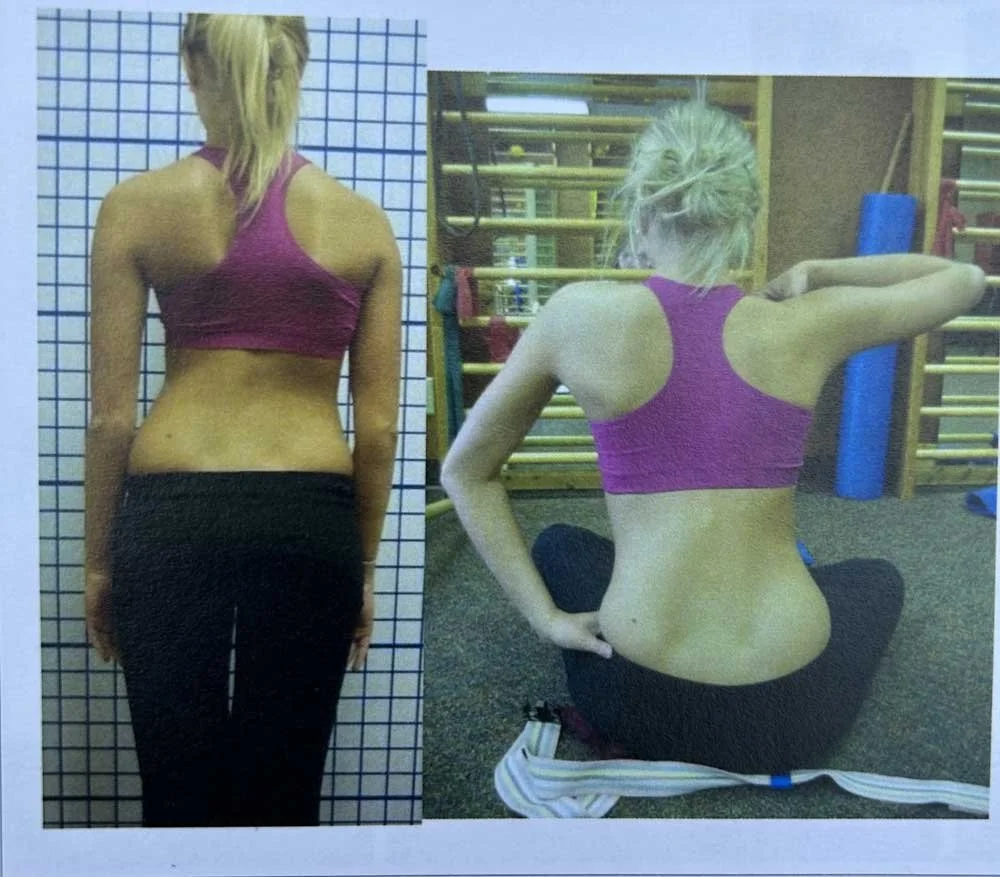
Schroth Postural Correction
Schroth Re-Posturing
The goals of PSSE, including the Schroth Method, are:
Improving the Scoliotic Posture
Halting Curve Progression
Improving Self-Image
Improving Quality of Life
Reduce Pain and Disability
Improve Vital Capacity (of the lungs)
The Schroth Method requires focus, determination and consistency. Those who are looking for a quick fix need not apply. Motor learning and changes to the central nervous system take time. Many, many hours of PSSE must be performed. The good news is that we work with “Schroth Rockstars” every day in our clinic, who are coming to us to learn, and replicating the scoliosis-specific exercises up to 5 times per week on their own, for 20-30 minutes each time. They are dedicated; and they are feeling and seeing results – just take a look at our before and after photos on our website. We hope you’ll become one of our Schroth Rockstars soon…
References:
1. Glavas J et al; Life. The Impact of Physical Activity on Adolescent Idiopathic Scoliosis. 2023: 13(5).
2. Burwell RG at al. Scoliosis. 2009; 4:24